Holiday Closure: Please note that our offices will be closed on December 24, 25 and 26, as well as on December 31, January 1 and 2. We wish you a wonderful holiday period and thank you for your understanding.
Holiday Closure: Please note that our offices will be closed on December 24, 25 and 26, as well as on December 31, January 1 and 2. We wish you a wonderful holiday period and thank you for your understanding.
Home Group Insurance FAQ
Choose one of the following sections to get more information.
These can be found on your insurance certificate, as well as your ID card, if you have Medical and/or Dental coverage.
If you do not have any of these documents, please contact your plan administrator. This information cannot be disclosed by our customer service agents.
Once you have completed your enrolment, your plan administrator will provide you with your certificate of insurance, which will include an identification card if you have Medical and/or Dental coverage. If this is the case, you can create your account on the My Humania claims platform, where you can also view and print your current ID card at any time, as follows:
To change your coverage or information, contact your plan administrator. Note that any family member you wish to add must meet the contract’s eligibility criteria.
You can also update your address as follows:
By email, at adm.coll@humania.ca. If you choose this option, be sure to clearly enter your policy/group and certificate/client numbers, name, old address and new address;
By calling our Customer Service team at 1-800-818-7236, Monday to Friday, from 8:00 a.m. to 5:00 p.m.
To find out who your beneficiaries are, you can contact the Customer Service Centre at 1-800-818-7236, Monday to Friday, between 8:00 a.m. and 5:00 p.m. or email your request to Be sure to clearly enter your policy and certificate numbers, your name and your employer.
To change your beneficiary designation, you must complete and sign the “Designation or change of beneficiary(ies)” form.
You can give it to your plan administrator or mail it to:
Humania Assurance Inc.
1555 Girouard Street West
Saint-Hyacinthe, Quebec
J2S 2Z6
The plan’s coverages are those retained by the policyholder. Participation in the plan is mandatory if you are eligible. You must contact your plan administrator for any changes to your coverage.
Your unique identifier, in HUM00000000000-00 format, is found on your ID card and allows health care professionals to submit claims directly on your behalf. You also need this identifier to connect to the My Humania online portal for the first time.
Be sure to present your ID card with your unique identifier to your professional. If they require assistance to process the claim, they may contact:
You can also pay the full fee at the professional’s office and submit your claim online with a copy of your original receipt for reimbursement.
You have three options to submit your claims:
You can check your coverage through your online account by following these steps:
Once you have accessed your My Humania account, in the “My health care and dental benefits” section, select “Consult my coverage.”
You have several options:
Depending on the option chosen, you may be prompted to select or enter additional information (e.g., the estimated expense amount).
Click the “Continue” button.
The estimated coverage amount will be displayed to the right.
For more information, click the “See details below” button under the results.
You can also view the coverage booklet your plan administrator can provide to you.
Lastly, you can call our Customer Service team at 1-800-818-7236, Monday to Friday, from 8:00 a.m. to 5:00 p.m.
The limit to reasonable and customary fees is a cost-control measure that is used by each insurer, but whose amounts may vary. This limit is used to prevent the plan from having to reimburse a non-standard fee for a service or item compared to the prices charged by most providers. The limit to reasonable and customary fees is therefore set so that the price charged by a majority of suppliers is fully eligible.
If a supplier charges an amount in excess of Humania Assurance’s reasonable and customary fee limit for a particular service/item, this means that the amount charged is greater than the majority of providers offering similar services. You will be required to pay the difference between the cost charged and the limit to the reasonable and customary charges for the service/item.
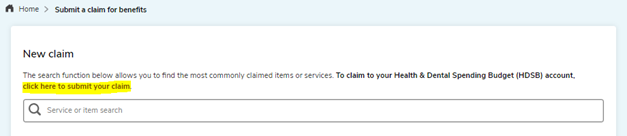
Here is the procedure:
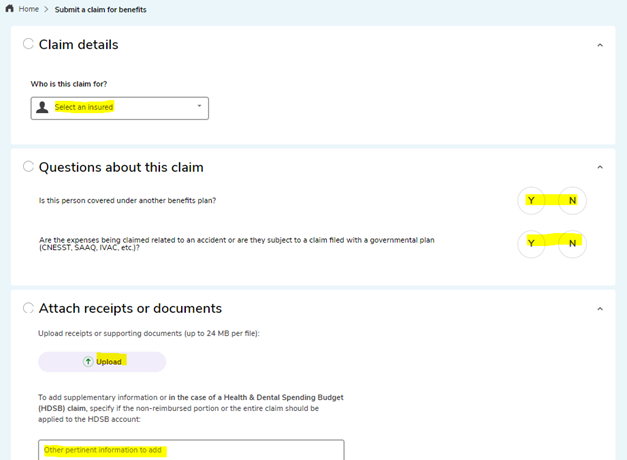
The application submitted will be processed by one of our claims analysts. Once processed, its status will be visible in My claims – View my history. You will also receive an email advising you that the treatment of your claim has been completed.
You can submit a claim online on My Humania for health care and dental benefits, excluding emergency costs outside your province of residence. If you have travel insurance coverage by Humania Assurance, you can contact customer service directly using the contact information on the back of your ID card.
Follow this procedure:
Sign in to access your My Humania account and click on your name, located at the top-right corner of the page.
Click “Change my email address” or “Change my password,” depending on the change you want to make, and follow the instructions on the screen
If you have forgotten your password, you can click on “Forgot your password?” on the My Humania home page and follow the instructions to reset your password.
If you enter an email address or password incorrectly multiple times, your account may be locked by the system. A message to that effect will appear. You will then need to contact our Customer Service team, who will be able to unlock the account for you after validating your identity by asking you questions about your account.
Most changes to your information must be communicated to us by your plan administrator, as they have an impact on plan management. That means you have to inform them of the changes. However, you can change your phone number through the following procedure:
You can sign up online by clicking on your name, then on the “My Humania account” section, and then under “Direct deposit.” You will be able to enter your financial institution’s branch, bank and account numbers.
To create a summary report of your claims, go to the “View my history” section from “My claims” and click on the “Report” link. From there, you can choose the types of fees you want to include and the period you need for your tax return. Please note that the history of your claims processed prior to November 1, 2023 is not available.
Make sure you have completed, attached and signed (as applicable) all sections of your disability claim:
Keep original documents for your records. Only the original Humania Assurance Standard Authorization is required.
You can submit your disability claim to us:
If you have short-term disability insurance coverage:
If you have long-term disability insurance coverage only:
Following the assessment of your claim, if you meet the definition of disability as well as the other clauses of your insurance contract, benefit payments will begin. Disability benefits are payable following the waiting period stipulated in your insurance contract. Payment frequency depends on your type of disability:
Requests for medical information considered in your disability claim may include:
It is your responsibility to stay in touch with your analyst throughout your disability claim.
You must inform your analyst of any changes to your medical condition throughout your disability claim.
You must also submit all medical (clinical notes, X-rays or specialist reports), financial (CNESST statement) or administrative (medical history form) documents requested by your analyst.
For more information on your responsibilities, refer to the Claimant’s Charter of Rights and Responsibilities.
It is our responsibility to inform you of the steps taken throughout your disability claim and to explain the decisions made.
It is also our duty to keep your personal and medical information confidential.
When you are fit to return to work, we will work with you and your health care professionals to find schedule and task accommodations, if necessary.
For more information on your rights, refer to the Claimant’s Charter of Rights and Responsibilities.
The policyholder must forward group insurance applications to the insurer or its representative within the time limits set out in the group insurance contract. The policyholder is responsible for the accuracy of the information provided during the application. Failure to meet the deadlines may result in the loss of the member’s rights in the event of a claim.
The policyholder is also responsible for deducting premiums and remitting them to the insurer on a monthly basis.
In the event of a claim submitted by a member, the member must provide the insurer with such information as is required for the consideration of the claim submitted.
It is the policyholder’s responsibility to ensure that all plan members and their dependents are eligible for coverage at the time they join. The policyholder must also ensure that this eligibility continues on an ongoing basis as long as members are covered by the group insurance contract. Eligibility standards and criteria are detailed in the contract in effect between the policyholder and Humania Assurance.
It is also responsible for providing members with their certificate of insurance as well as with a copy of the brochure detailing the coverage available to them.
The policyholder also has a duty to inform the members with regard to the group insurance contract. However, it cannot provide advice to the members. It must refer them to their insurer or its representative when a request exceeds its duty to inform.
Watch the explanatory video.
The normal period for submitting an application or a change affecting a member’s file is 30 days. However, this period may vary from one contract to another. The policyholder must refer to their contract in the GENERAL CONDITIONS section under Responsibilities of the policyholder to determine the period that applies. Failure to meet the deadline may result in the loss of the member’s rights in the event of a claim.
The insurer must be notified of layoffs and leave without pay within the time limits set out in the contract, as these situations may impact the member’s benefits and rights in the event of a claim. The deadline is the same as for any notice submitted to the insurer to change a member’s file and is found in the GENERAL CONDITIONS section under Responsibilities of the policyholder.
You must complete and sign the “Pre-authorized Debit Agreement” form and forward it to us with a copy of your void cheque.
Humania Assurance Inc.
1555 Girouard Street West
Saint-Hyacinthe, Quebec
J2S 2Z6
By fax at 450-773-1809
You can contact our Customer Service team Monday to Friday from 8 am to 5 pm., at 1-800-818-7236.
Customer Service, group insurance:
The email address for group insurance Customer Service team is groupservice@humania.ca.
Make sure to clearly indicate your policy numbers and your name.
You will receive a response within 2 to 3 business days.
To submit a health care and/or dental benefits claim:
First, you can complete the claim online.
Alternatively, on the Make a claim page, select the type of claim you wish to make, then follow the steps requested.
The e-mail address is health.claims@humania.ca .
You can send mail to Humania Assurance:
1555 Girouard Street West
Saint-Hyacinthe, Quebec
J2S 2Z6